If you’ve been dealing with relentless bloating, gas, or nausea even after being told your labs are “normal” this story might feel a little too familiar. Despite following a “clean diet” and trying everything from endoscopies to elimination plans, this high-performing executive still felt off: daily discomfort, sulfur-smelling gas, brain fog, and a cough no one could explain. The surprising culprit? An infection he had already tested negative for: H. pylori.
Client J Overview
Main Symptoms: Chronic nausea (5/5), belching (5/5), gas (5/5), fatigue (5/5), chronic coughing (5/5), GERD symptoms, sulfur smelling gas and loose stools.
History:
- Post-COVID onset of gut issues (nausea, vomiting, coughing, fatigue)
- Previous testing: endoscopy, imaging, digestion study — all “normal.”
- Previously negative for H. pylori on testing
Impact: Symptoms affecting energy, family life, and professional performance despite “exceeding expectations” at work.
Medications: Bupropion for anxiety/depression.
Diet/lifestyle: Whole30 brought some relief, but not sustainable; high stress (rated 9/10 for work).
Why Was He Bloated, Nauseous, and Drained Even After Normal Tests?
Despite years of digestive discomfort and “normal” conventional testing, Client J’s functional stool and mineral testing revealed several red flags that helped explain every single one of his symptoms — from nausea and belching to sulfur-smelling gas, fatigue, and chronic coughing.
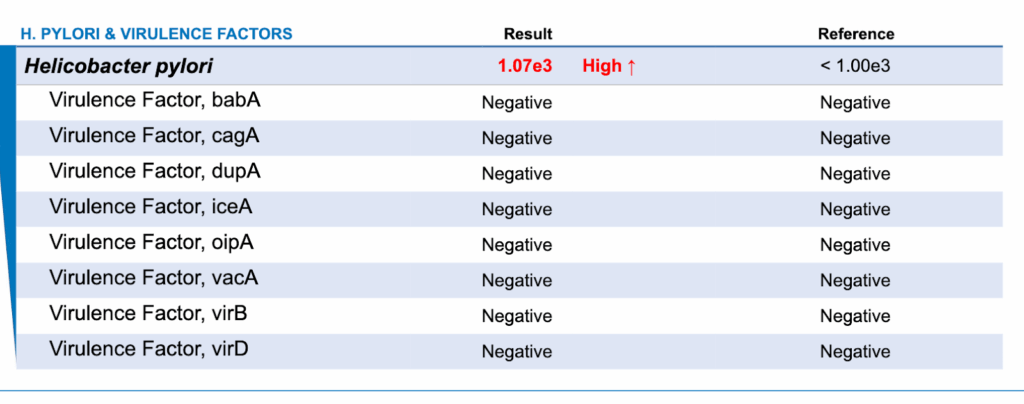
H. pylori: The Missing Piece
Although previous testing had ruled out H. pylori, this advanced stool analysis revealed a positive result. H. pylori is known to suppress stomach acid, which can lead to:
- Poor protein digestion
- Increased belching and upper GI discomfort
- Sulfur-like gas (due to fermentation and bacterial overgrowth)
- Chronic coughing, a lesser-known symptom often tied to silent reflux and upper GI irritation
Even though no virulence factors were detected, his levels were high enough to significantly disrupt digestion and nutrient absorption — which also has downstream impacts on mineral levels and stress patterns (more on that below).
Low Levels of Keystone Bacteria
Beneficial species like Akkermansia muciniphila and Faecalibacterium prausnitzii were far below optimal. These bacteria support gut lining integrity and immune balance. Their depletion makes the gut more reactive to food, infection, and stress.
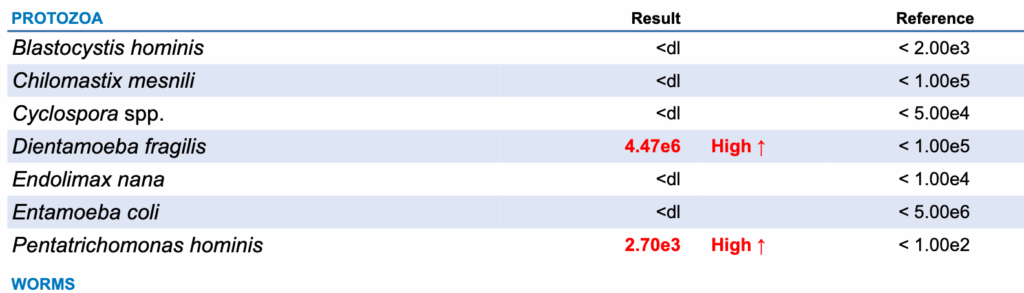
Gut Overgrowth + Infections
He had a constellation of unwanted microbes contributing to inflammation, bloating, and loose stools:
- Streptococcus spp. – Elevated
- Candida spp. – Detected
- Dientamoeba fragilis and Pentatrichomonas hominis – Parasitic infections
- Desulfovibrio spp. – High end of normal; known for producing sulfur-smelling gas
Impaired Gut Immune Function + Inflammation
- Low Secretory IgA (sIgA): Suppressed gut immunity, making him more vulnerable to pathogens and food reactivity
- Elevated Calprotectin: Clear sign of gut inflammation
- Steatocrit Present: Indicating mild fat malabsorption — a likely contributor to his loose stools and fatigue

HTMA: A Body Stuck in Survival Mode
Mineral testing (HTMA) showed that Client J was in a “4 Lows” pattern — low in calcium, magnesium, sodium, and potassium. This is a metabolic burnout pattern that reflects:
- Mineral depletion from long-term stress
- Poor digestion and absorption (including of minerals)
- Dysregulated adrenal and thyroid function
Despite small burps on his baking soda test, the combination of low stomach acid symptoms, H. pylori infection, and very low cobalt strongly suggested absorption issues.
We also noted:
- High Na/Mg and Zn/Cu ratios → indicating adrenals on high alert (fight or flight mode)
- Hyperthyroid-type output patterns → fatigue followed by crashes, poor stress tolerance
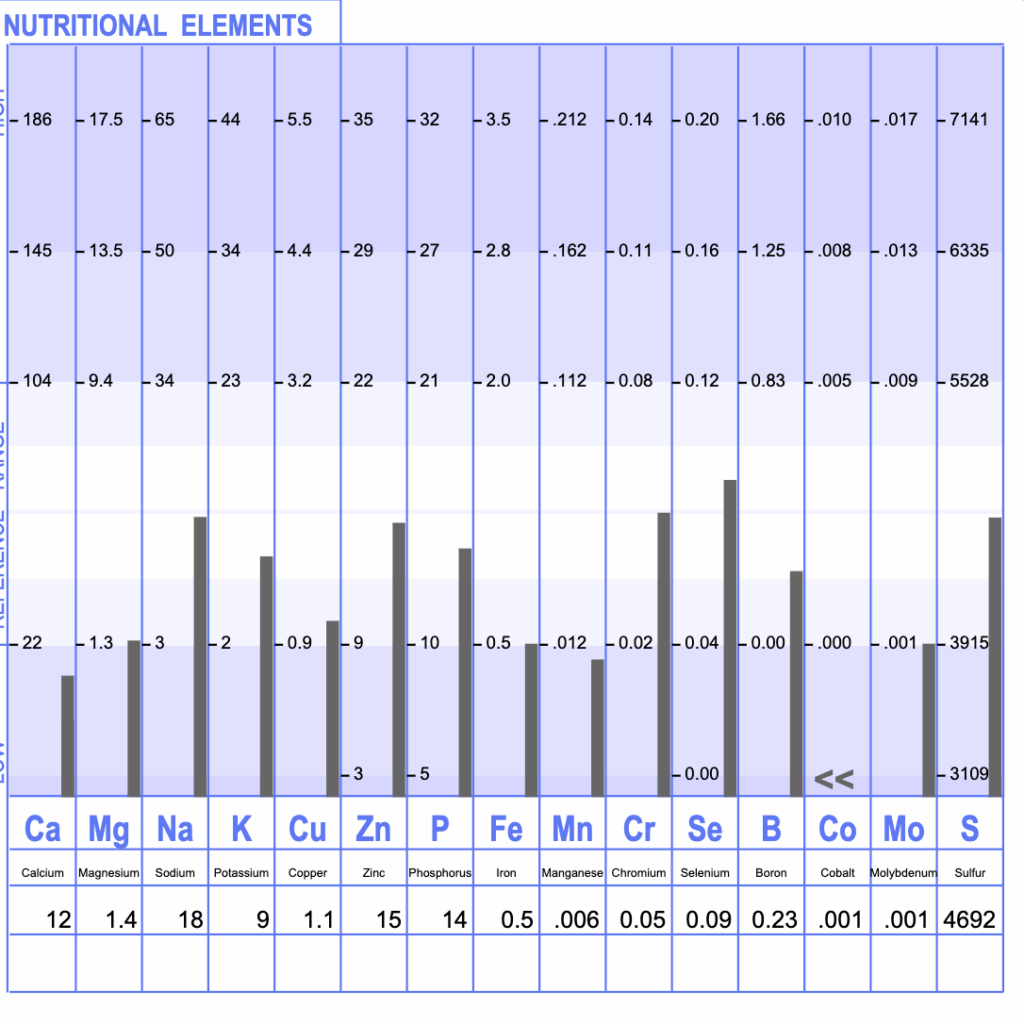
H. pylori often contributes to 4 Lows because low stomach acid impairs protein breakdown and mineral absorption — especially B12 (cobalt), zinc, and iron — keeping the body in survival mode even if eating a healthy diet.
Root Causes Identified
Client J’s symptoms weren’t “just in his head.” They stemmed from a perfect storm of:
- Undiagnosed H. pylori infection
- Gut microbial imbalances (low beneficial bacteria + opportunistic overgrowth)
- Parasitic infections + yeast
- Inflamed and under-functioning gut lining
- Severe mineral depletion and chronic stress response
- Contributing lifestyle factors: high stress, overeating, dehydration, poor meal composition
The 5 Systems We Targeted (Step-by-Step)
1. Digestive Secretions (Stomach Acid, Bile, Enzymes)
➡ Goal: Improve how his body breaks down food so it stopped fermenting and triggering symptoms.
- Nutrition
- Structured meals with protein, fat, fiber, and color
- Added protein and fat to carbs to slow transit and ease digestion
- Lifestyle
- Reduced fluid intake with meals
- Emphasized chewing and slow, undistracted eating
- Targeted Support (phased in)
- Digestive bitters to naturally stimulate stomach acid
- Betaine HCl to increase acid levels where appropriate (after H pylori was addressed)
- Bile flow support with taurine and bile salts
- Herbal support for stomach lining and H. pylori (e.g., mastic, deglycyrrhizinated licorice, zinc carnosine)
- Immunoglobulins and yeast-based probiotics to bind toxins and support microbial balance
2. Mineral Status (Potassium, Sodium, Magnesium, Cobalt)
➡ Goal: Rebuild his depleted mineral stores and stabilize energy, digestion, and stress response.
- Nutrition
- Increased intake of magnesium-rich foods (e.g., pumpkin seeds, greens, oats)
- Used mineral rich salt on meals for sodium balance
- Structured meals using our PFFC framework to stabilize blood sugar and reduce nutrient depletion
- Lifestyle
- Hydration with minerals, not just plain water
- Gradual improvements in sleep, movement, and recovery
- Targeted Support
- Custom mineral powder including magnesium, potassium, sodium, and trace minerals
- Phased out additional magnesium as levels improved with his custom blend to decrease supplement load
3. Motility
➡ Goal: Normalize loose stools and reduce gas by calming the gut and correcting overgrowth.
- Nutrition
- Meal timing every 3.5–4 hours to support motility waves
- Combined protein and fat with carbs to slow digestion
- Lifestyle
- Focused on meal spacing, walking, and meal hygiene to support gut rhythm
- Targeted Support
- Herbal antimicrobials to reduce bacterial overgrowth and parasites
- Spore-forming and S. boulardii probiotics to support immune response and motility
- Continued immunoglobulin therapy to bind and remove microbial byproducts
4. Detox & Elimination Pathways
➡ Goal: Support the liver and bowels so toxins could move out instead of backing up and worsening symptoms.
- Nutrition
- Focused on cruciferous vegetables and fiber-rich meals
- Emphasized cooked, easy-to-digest detox-supportive foods
- Lifestyle
- Promoted sweating, movement, and deep breathing
- Improved sleep to enhance overnight detoxification
- Targeted Support
- Liver support herbs (e.g., milk thistle, dandelion root)–> we added these to his custom blend to also decrease supplement load and make it super easy to be consistent
- Taurine and bile acid support to enhance fat digestion and elimination (also added to his custom mineral blend to help with supplement load and consistency)
- Binders (humic/fulvic acid and zeolite) to support toxin clearance
- Oral microbiome rinse to reduce microbial H Pylori load upstream
5. Gut-Brain-Nervous System
➡ Goal: Reduce stress signals in the gut so digestion could work efficiently and energy could stabilize.
- Nutrition
- Prioritized protein-rich snacks and meals to stabilize blood sugar
- Removed artificial sweeteners and reactive additives
- Lifestyle
- Daily stress relief: meditation, prayer, journaling
- Focused sleep hygiene to support nervous system recovery
- Emphasized quality rest (even with toddler interruptions)
- Targeted Support
- Nervous system minerals (magnesium, potassium, sodium)
- Nutrients depleted by medication (e.g., B vitamins, magnesium, CoQ10)
This plan unfolded slowly over six months, with each step introduced based on how his body was responding. That’s the difference between a supplement-heavy plan… and a true root-cause approach.
His Transformation (In Just a Few Months)
After years of feeling like his symptoms were “in his head,” Client J finally had a clear, phased plan that didn’t rely on restriction or guesswork — and the results speak for themselves.
Here’s what shifted:
- Diarrhea improved from 6/10 to 2/10
- Bloating reduced from 5/10 to 1/10
- Sulfur-smelling gas completely resolved
- Chronic nausea nearly gone
- Persistent cough improving — a sign of healing reflux
- Mental clarity and energy returning after feeling foggy and drained for years
- Confidence with food increased — no longer afraid of what might trigger symptoms
All of this happened without extreme restriction — just the right support, at the right time.
Client J was also able to resume a more normal daily rhythm, with improved digestion allowing him to feel more present with his family and more energized at work. As a high-performing executive, this transformation wasn’t just about symptom relief — it was about getting his life back.
“I feel clearer, calmer, and more in control. This is the best I’ve felt since before COVID.”
Key Takeaways
Client J’s case is proof that bloating, gas, and gut issues aren’t always about what you eat — they’re about how your body is functioning. In his case, previously undetected H. pylori, mineral depletion, and gut inflammation were driving symptoms that no amount of clean eating could solve.
By addressing the 5 core systems that impact digestion — not just gut bugs or food triggers — we helped him finally feel like himself again.
And most importantly, this all happened with a sustainable plan that fit into his busy life as a successful executive, without adding more stress or restriction.
Want Help Like This?
If you’re tired of hearing “everything looks normal” while still feeling anything but, the gutTogether® team is here to help.
✨ Here’s how to get started:
- Click here and navigate to the “book a discovery call” button
- Fill out your application so we can understand your symptoms and health history
- If it’s a good fit, we’ll set up your free call to walk through next steps
Your body is capable of healing — when you give it what it actually needs.

