You’re bloated by the end of the day, constipated for days at a time, or so exhausted you can barely drag yourself out of bed. You’ve had the colonoscopy, the bloodwork, maybe even an endoscopy, and everything came back “normal.” But nothing about how you feel is normal.
So now you’re left wondering “what’s my next step?” Could a GI Map stool test finally explain what’s going on?
Why a Colonoscopy Isn’t the Whole Story
Here me when I say this: A colonoscopy is an incredible, lifesaving tool. It rules out structural disease like cancer, polyps, and IBD. If you’re over 45, have bleeding, or a strong family history, it’s non-negotiable. But here’s the limitation: a colonoscopy tells you what your gut looks like, not how it’s functioning. That’s why so many people leave with “normal” results but still don’t feel normal.
That’s where advanced stool testing like the GI Map comes in. Instead of only showing structure, it looks at how your gut is actually working day to day. It answers the question a colonoscopy can’t: why do you still feel bloated, constipated, or exhausted when everything looks fine on paper?
What the GI Map Actually Measures
The GI Map (Gastrointestinal Microbial Assay Plus) uses DNA technology to map your gut function. Instead of just asking “is there something dangerous here,” it asks “is your digestive system actually working?” You don’t have to settle for a vague IBS diagnosis and “learn to live with it”: the GI Map helps uncover what’s really driving your symptoms.
It looks at:
- Pathogens and parasites like H. pylori or Giardia
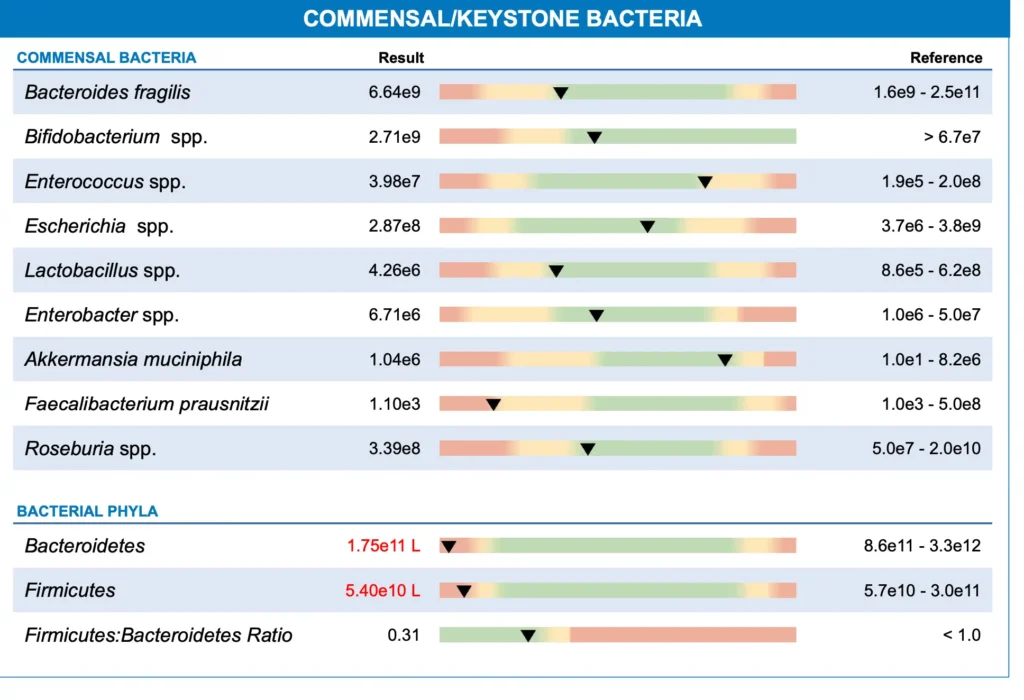
- Beneficial bacteria that keep your gut lining strong
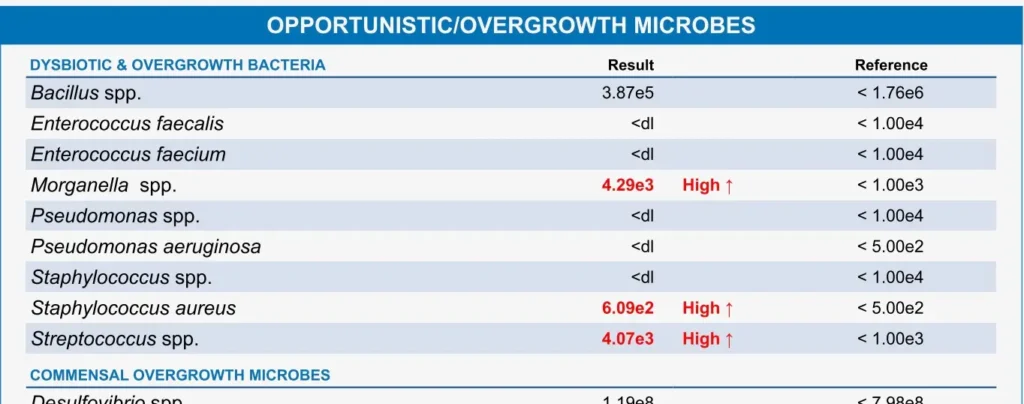
- Opportunistic bacteria that flare under stress or antibiotics
- Digestive enzymes and fat absorption markers
- Gut immune function through secretory IgA
- Inflammation markers like calprotectin
- Detox pathways such as beta glucuronidase, which link gut and hormone health
Real-Life Results: What a GI Map Can Show
One client I’ll call Rachel had multiple colonoscopies, scopes, and endless lab work. Everything was “normal.” Yet she was still so constipated she needed suppositories, bloated daily, and dragging herself out of bed.
The GI Map revealed low stomach acid, gut bacterial imbalances (including too few GOOD bacteria), and a parasite which were all missed by standard testing. Once we had this data, we created a plan that finally worked (including nutrition, lifestyle and supplementation to address her specific concerns).
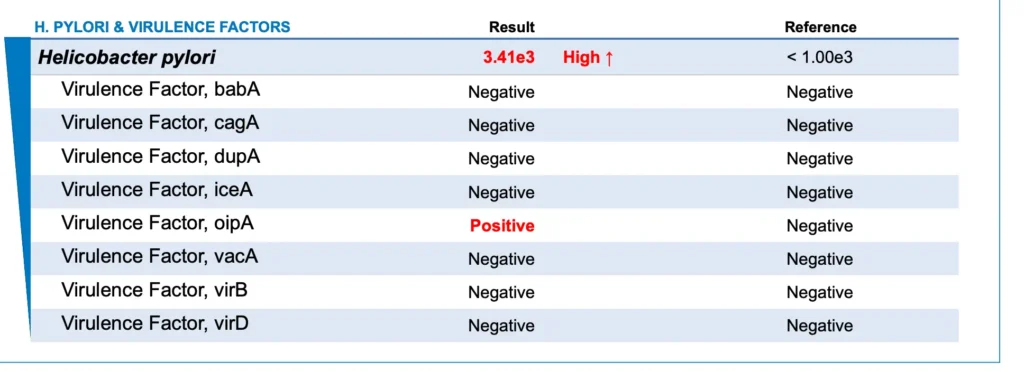
Another client had been on PPIs for years, cycling through higher and higher doses with no relief from reflux. She felt trapped because every doctor visit ended with the same recommendation: “just keep taking the medication and increase your dose.” But deep down she knew this wasn’t fixing the problem. Her GI Map told a completely different story.
It revealed H. pylori, a bacteria known to lower stomach acid. This explained why food felt like it sat in her stomach like a brick, triggering the reflux she couldn’t get rid of. It also showed poor fat digestion, a sign of sluggish bile flow that can lead to nutrient deficiencies and further digestive stress.
On top of that, her beta glucuronidase was elevated, which meant her body was recycling estrogen instead of clearing it. Suddenly, her stubborn acne, heavy periods, and mood swings made sense too.
By addressing these root causes and supporting stomach acid, improving bile flow, and lowering beta glucuronidase, her reflux finally calmed down. But the changes didn’t stop there. Her skin cleared, her periods became lighter and less painful, and even the recurring UTIs she thought were unrelated stopped coming back. What she once thought were separate, random issues were all connected, and the GI Map helped piece the puzzle together.
Do I Need Both: GI Map or Colonoscopy?
The short answer: sometimes both, but for different reasons. A colonoscopy rules out disease. A GI Map explains dysfunction. If you’ve had a normal colonoscopy but your symptoms continue, that’s exactly where the GI Map shines.
The other benefit of the GI Map is that it’s non-invasive and can often help determine if a colonoscopy is even necessary in the first place. If you don’t have red flag symptoms like bleeding, unexplained weight loss, or a strong family history of colon cancer, a GI Map can be a powerful first step. It can highlight patterns of inflammation, immune stress, or digestive dysfunction that might explain your symptoms without immediately jumping to a scope. And if the results do suggest something more serious could be going on, that’s when a colonoscopy becomes the logical next step.
In that way, the GI Map and colonoscopy work hand in hand: one rules out disease, the other uncovers dysfunction. Together, they make sure you’re not just told “everything looks fine” when clearly it doesn’t feel fine.
When the GI Map Is Worth It
If you’ve tried everything: medications, restrictive diets, supplements and you’re still stuck with symptoms, the GI Map can help connect the dots.
It’s especially useful if you’re dealing with:
- Bloating or constipation that hasn’t resolved with fiber, laxatives, or multiple gut protocols
- Reflux despite PPIs or antacids, where medication only masks symptoms without fixing the root cause
- Hormone issues like PMS, acne, or heavy cycles with little improvement from diet elimination, topicals or medications
- Autoimmune or thyroid conditions with flare-ups that don’t make sense even when your labs are “stable”
- Food sensitivities that keep growing, leaving you afraid to eat because your list of “safe” foods feels smaller by the week
- Chronic fatigue with “normal” labs, where doctors say everything looks fine but you still feel drained and unable to function
The truth is, these symptoms usually aren’t random and they’re connected through your gut, and the GI Map is often the first test that shows how everything ties together.
Your Next Step After A Normal Colonoscopy
If your colonoscopy was normal but you’re still miserable, the GI Map may be the missing piece. It won’t replace a colonoscopy, but it can give you answers about function that no scope or standard stool test can provide.
Think about the symptoms you’ve been told to “just live with”: the daily bloating that makes you look six months pregnant, constipation that leaves you uncomfortable and sluggish, reflux that keeps you up at night, or even acne, PMS, and heavy periods that don’t get better no matter how many medications or diets you try. These aren’t random issues. They’re often connected through patterns in your digestion, immune system, and gut bacteria.
To date, I’ve run over 1,500 GI Map tests, and I’m still amazed at how consistently the same themes show up: low stomach acid, sluggish bile flow, depleted good bacteria, or high beta glucuronidase recycling estrogen. Each test tells a story and shows us why you feel the way you do. This is why I always say we want to test, not guess. Without that data, you’re stuck throwing supplements or diets at symptoms. With the data, you finally have a roadmap and you will feel better faster.
You don’t have to keep guessing. If you’re ready for clear answers, you can start with a Gut Health Audit to find out if GI Map testing is the right next step. Or, if you know you’re ready for comprehensive support, apply for gutTogether, my six-month 1:1 program where GI Map testing is part of your personalized plan.








